A series of studies has shown that the connective tissue surrounding our cells plays a very active role in human health and disease
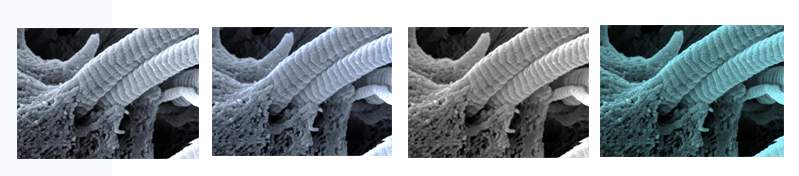
The “cushy” material that surrounds the cells in our tissues – collagen, gelatin and laminin, collectively known as extracellular matrix (ECM) – is the connective tissue that gives our organs shape and structure. A series of studies in the lab of Prof. Irit Sagi of the Weizmann Institute of Science’s Biological Regulation Department is revealing that this tissue is much more than scaffolding and packing, and its malfunctions may play a role in diseases, from the sniffles to cancer.Sagi explains that if it was once thought of as merely structural, today’s research shows that the ECM contains a reservoir of information molecules that are continuously processed by enzymes outside the cells. Within the ECM, there are two “opposing” groups of enzymes busily acting on the tissue. One, the proteases, are cleavers that chop proteins and fibers so that the cells can pass through. The other, lysyl oxidases, stitch together the collagen molecules in the tissue and are active, for example, in tissue regeneration.
Cleaving leaves marks
Cleaving and sealing are both necessary, of course, in the normal functioning of the body, but the processes must be carefully regulated, including “decommissioning” the enzymes once they finish their work. “The problem,” says Sagi, “is that in the immune response or inflammation, unregulated cleaving can lead to an excess of signaling molecules being released from the connective tissue. And cancer cells may manage to equip themselves with protease ‘scissors’ and cut their way out of the tissue, which is the first step to malignancy.”
The first study, published in the Proceedings of the National Academy of Science (PNAS), investigated how the connective tissue is damaged by excessive protease activity. The cleaving enzymes leave their individual marks on the tissue they cut, and the resulting physical changes reshape the ECM proteins and cause the release of further signaling molecules stored in the connective tissue. This work was done together with Prof. Ido Amit of the Weizmann Institute’s Immunology Department, and Prof. Hideaki Nagase of Oxford University.

Next, with results that were published in the Journal of Experimental Medicine, Sagi and her colleagues looked at the involvement of immune cells called macrophages in the building of connective tissue in tumors. Using mouse models of intestinal cancer, they found heightened activity of the “sealing” enzymes, which, in the presence of macrophages, increased their pace and created thick, fibrous tissue – the supporting structure for cancer cells. When the researchers, including Prof. Chen Varol and Dr. Tamar Geiger of Tel Aviv University, kept certain immune cells from reaching the tumors, they managed to block collagen buildup, and the rate at which the cancer cells spread was significantly slowed.
In a study published in Cancer Research, conducted together with the group of Prof. Yosef Yarden of the Institute’s Biological Regulation Department, the researchers developed an antibody that reinstates the regulation of the sealing enzyme’s activity. In models of breast cancer, among other things, this antibody slowed tumor cell proliferation and metastasis to the lungs.
Double damage
Finally, a study published in Host & Microbe Cell focused on damage to the connective tissue in the lungs when disease strikes twice. In some cases of flu, pneumonia bacteria take advantage of damage that is already done to the lung tissue to mount a new invasion, compounding the destruction and causing severe illness. In mice infected with both virus and bacteria, the scientists, including members of Amit’s group, noted that one particular cleaving enzyme, called MT1-MMP, was out of control. The study suggests that treatments to prevent connective tissue damage by blocking the activities of this particular enzyme could lessen the chances of opportunistic infections like pneumonia.
Among other things, this antibody slowed tumor cell proliferation and metastasis to the lungs
“All these studies show that the packing material that holds our cells in place is so much more than mere ‘scaffold’,” says Sagi. “The remodeling that takes place in the extracellular matrix in health and disease makes it more than a just a bystander—it’s a ‘partner in a crime.’ The more we understand about its function in health and disease, the more we will be able to use that knowledge to develop therapeutic agents and possibly, in the future, the means to protect and regulate it to slow or stop disease progression.”
Prof. Irit Sagi’s research is supported by the Rising Tide Foundation; the Leonard and Carol Berall Post Doctoral Fellowship; the Spencer Charitable Fund; the Leona M. and Harry B. Helmsley Charitable Trust; and the Azrieli Foundation. Prof. Sagi is the incumbent of the Maurizio Pontecorvo Professorial Chair.
Recent Comments